Every day, patients come to our practice with concerns about their cholesterol levels, particularly elevated LDL cholesterol. They’re often worried about their risk for heart disease. They may be already taking a statin to lower their cholesterol, or they’re concerned about whether they should start one.
This fixation stems from long standing myths about heart disease—myths rooted deeply in our history since the post-WWII era, when big food corporations began pushing carbohydrates while demonizing fats for profit.
 After World War II, the U.S. saw a dramatic shift in dietary patterns, encouraged by large food corporations that promoted processed, shelf-stable foods. This era marked the beginning of a strategic demonization of fats—particularly saturated fats—in favor of carbohydrates.
After World War II, the U.S. saw a dramatic shift in dietary patterns, encouraged by large food corporations that promoted processed, shelf-stable foods. This era marked the beginning of a strategic demonization of fats—particularly saturated fats—in favor of carbohydrates.
Recognizing that a low-fat diet would naturally lead people to consume more carbohydrates, sugar executives devised a strategy. They anticipated that dietary habits would pivot towards carbohydrates by about 20 percent, which would greatly benefit all carbohydrate-related industries [1]. To ensure this shift, in 1967, these executives funded Harvard scientists to produce a review that downplayed the harmful effects of sugar and instead implicated fats and cholesterol as the primary culprits of heart disease [1].
This manipulation of science was not isolated to the sugar industry; the vegetable oil and other carbohydrate-centric industries also played significant roles, profiting immensely from the increased consumption of their products as public health declined. Now, half a century later, diabetes and obesity among children and adults have skyrocketed.
Heart disease is not merely about high cholesterol or saturated fat intake. The real culprit is often the health of the blood vessels themselves, specifically the endothelial cells lining them [2]. You can think of endothelial cells like single-cell tiles lining the inner walls of your blood vessels. Covering these cells is a slippery, damage-repellent layer called the glycocalyx. The glycocalyx works like the slippery scales on a fish, making the interior of your blood vessels an efficient pathway for blood to flow through [2].
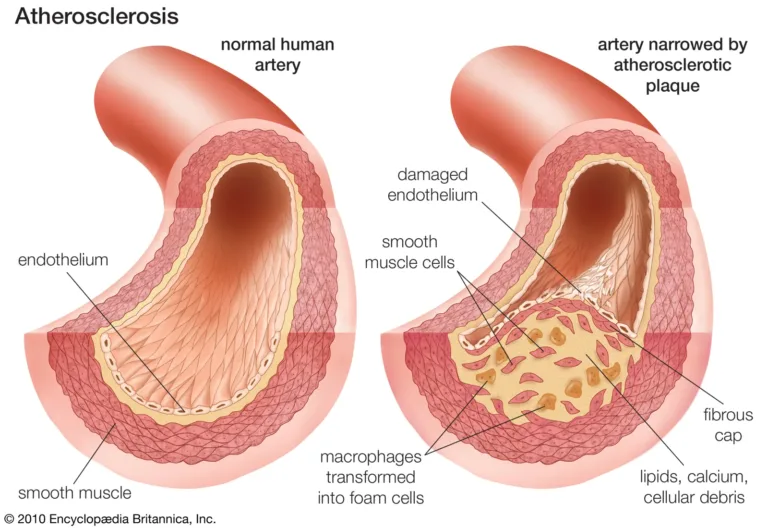
Damage to the glycocalyx and endothelial cells beneath leads to blood clots. This is our bodies’ way of sealing up the cracks to prevent us from bleeding out. However, these clots are meant to be controlled in size and eventually shaved down once stabilized. Problems start to occur when damage to our cells outpaces our ability to repair them. The result is the buildup of atherosclerotic plaques, narrowing arteries and potentially leading to heart attacks [2].
Cholesterol is a complex molecule crucial for hormone production and cellular structure. It is transported in the body by lipoproteins, which include LDL (low-density lipoprotein) and HDL (high-density lipoprotein). LDL, often misleadingly labeled as “bad” cholesterol, carries cholesterol from the liver to other parts of the body. HDL, commonly known as “good” cholesterol, helps transport cholesterol from the body back to the liver for processing and elimination.


It was once believed that high LDL levels would lead excess cholesterol to build up on the walls of blood vessels and therefore cause the cascade of calcification leading to atherosclerosis. However, this is not entirely accurate.
The actual precursor to heart disease is inflammation that weakens and damages the blood vessel walls [3]. This endothelial damage is often caused by metabolic disorders like diabetes and high blood sugar, chronic infections such as Chlamydia Pneumoniae, smoking cigarettes, heavy metal toxicity, and high blood pressure [4,2]. These factors can cause LDL to accumulate where endothelial damage already exists, worsened by phagocytes that adhere cholesterol to these vulnerable areas [3].
Additionally, research shows that high LDL levels are often a response to underlying metabolic and immune disorders [5]. Cholesterol can accumulate in macrophages and other immune cells, promoting inflammatory responses in an effort to neutralize or contain the threat. This response is initially beneficial; however, when this mechanism becomes chronic or unbalanced, it can contribute to the development of atherosclerosis in a vicious cycle [5].
Instead of addressing these root causes, conventional approaches often focus solely on reducing cholesterol levels. This overlooks crucial underlying factors such as chronic infections, metabolic disorder, and toxin exposure, and often can create new problems for patients as well.
Statin drugs are widely prescribed to lower cholesterol as a strategy to reduce the risk of heart disease. They work by inhibiting a key enzyme in the liver responsible for cholesterol production, effectively lowering levels of LDL cholesterol. However, emerging research challenges the robustness of these benefits. Studies indicate that while statins do effectively lower LDL cholesterol, this does not always translate into a significant reduction in cardiovascular events [6]. In fact, they do not prevent heart disease in 98.8% of patients [6]. This discrepancy raises questions about the universal effectiveness of LDL reduction as a preventive strategy and lifestyle medicine.
 Moreover, statins can disrupt the synthesis of Vitamin K2, a crucial nutrient for cardiovascular health. K2 activates the Matrix GLA Protein (MGP) which prevents the calcification of blood vessels, thereby maintaining their flexibility [7]. It also plays a key role in regulating calcium deposition, ensuring calcium is directed to the bones rather than accumulating in the arteries. The inhibition of Vitamin K2 synthesis by statins can lead to increased arterial stiffness and contribute to cardiovascular risk, contrary to their intended use [8].
Moreover, statins can disrupt the synthesis of Vitamin K2, a crucial nutrient for cardiovascular health. K2 activates the Matrix GLA Protein (MGP) which prevents the calcification of blood vessels, thereby maintaining their flexibility [7]. It also plays a key role in regulating calcium deposition, ensuring calcium is directed to the bones rather than accumulating in the arteries. The inhibition of Vitamin K2 synthesis by statins can lead to increased arterial stiffness and contribute to cardiovascular risk, contrary to their intended use [8].
There are also concerns about the broader impacts of artificially lowering cholesterol levels. As we discussed, cholesterol is essential for cell membrane structure and the production of certain hormones. Excessively low cholesterol, driven by statin use, can be associated with cognitive decline including dementia, hormone imbalances, and other health complications [9].
Adding complexity, the shifting laboratory reference ranges for LDL cholesterol, influenced by the widespread use of statins, have altered what is considered “normal.” As more people use statins, the average LDL levels decrease, shifting the lab reference ranges downward. This shift can lead to overdiagnosis of high cholesterol in individuals who, under previous standards, would have had normal LDL levels.
For a deeper understanding of lab reference ranges and interpreting results, you can read more on our blog: Beyond Normal: Understanding Your Lab Results.
In our clinic, we take a holistic approach to heart health and reducing cardiovascular risk, recognizing that inflammation from certain disease states and conditions plays a significant role in cardiovascular risk. Our comprehensive biomarker assessments establish baselines for all patients, measuring not just typical lipid panels but also metabolic markers like:
We also assess markers for inflammation and blood flow, such as:
Another essential lab is assessment for hidden, chronic infections like Chlamydia Pneumonia which can contribute to atherosclerosis [4].
To ensure our patients receive essential nutrients for heart health and bone strength, we recommend a daily vitamin A, D, and K complex, with particular attention to Vitamin K2. This approach helps prevent calcium from contributing to arterial plaque, directing it instead towards strengthening bones. Osteocalcin is another key biomarker we measure, as it can tell us truly how healthy your bones are. While bone density tests measure the quantity of bone, osteocalcin levels indicate the actual biological activity. We use this marker to guide our patients away from misguided, potentially harmful calcium supplements and encourage dietary sources of K2 with appropriate supplementation.
Additionally, we discuss the importance of a balanced diet, emphasizing the right macronutrient balance and debunking myths about fat intake. We encourage our patients to follow their blood type diet and fill their plates with more whole foods and leafy greens in lieu of processed carbohydrates and vegetable oils.
For those on statin therapies, we explore alternatives like Red Yeast Rice and other natural compounds that can lower LDL cholesterol without the side effects associated with statins. Our goal is to support the body’s natural processes through proper nutrition and informed choices about treatments.
 Understanding cardiovascular health extends beyond the simple metrics of LDL cholesterol and dietary fat intake. It’s about supporting the body’s natural processes with the right nutrients and making informed choices about medical treatments. We encourage our patients to adopt a holistic view of their health, focusing on true indicators of cardiovascular well-being and ensuring their bodies are supported with the necessary nutrients for optimal health.
Understanding cardiovascular health extends beyond the simple metrics of LDL cholesterol and dietary fat intake. It’s about supporting the body’s natural processes with the right nutrients and making informed choices about medical treatments. We encourage our patients to adopt a holistic view of their health, focusing on true indicators of cardiovascular well-being and ensuring their bodies are supported with the necessary nutrients for optimal health.
Ready to take control of your heart health? Schedule a consultation with us today!
References:

Lilly Young, raised in the realm of health and wellness by her mother, Dr. Lari Young, blends her passion for writing and medical research to offer insightful contributions to the MyHealth1st blog.

Join our newsletter for health news and My Health 1st events.