How Thermography Works
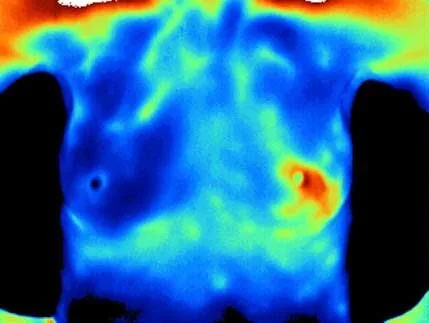
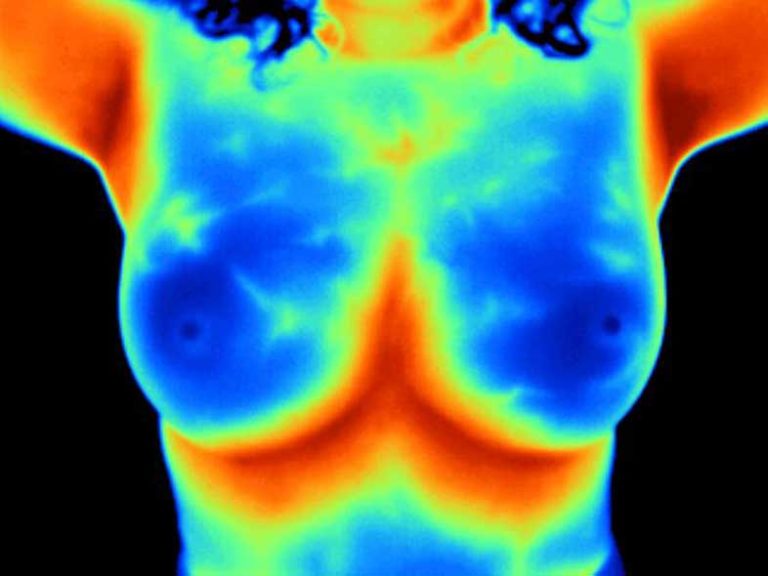
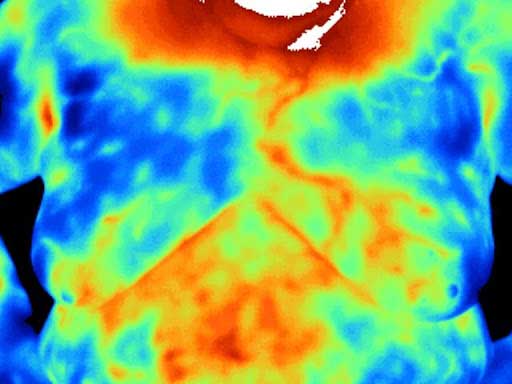
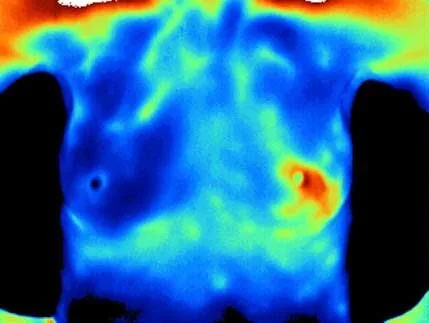
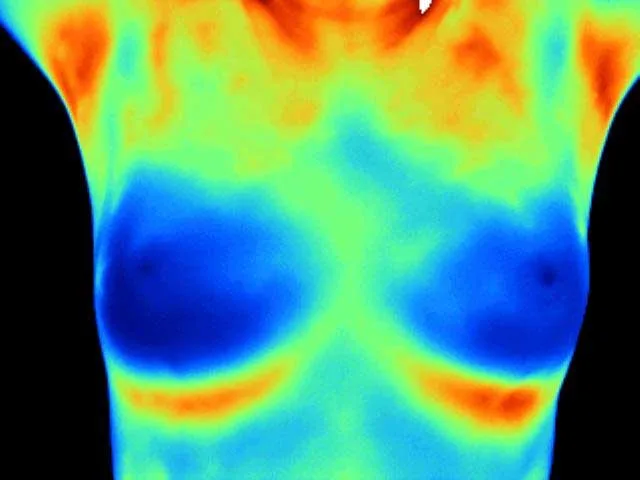
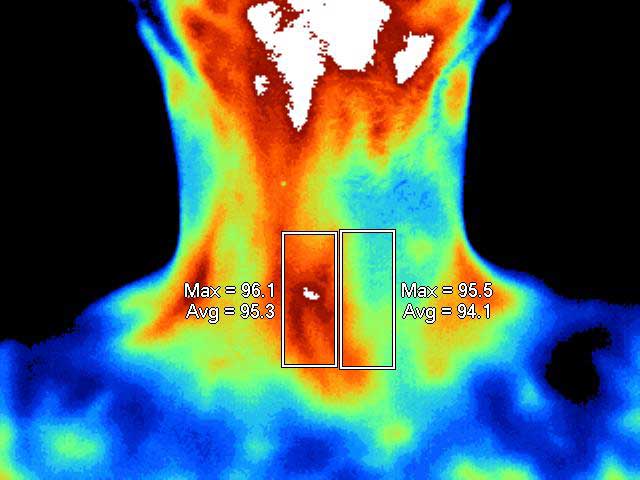
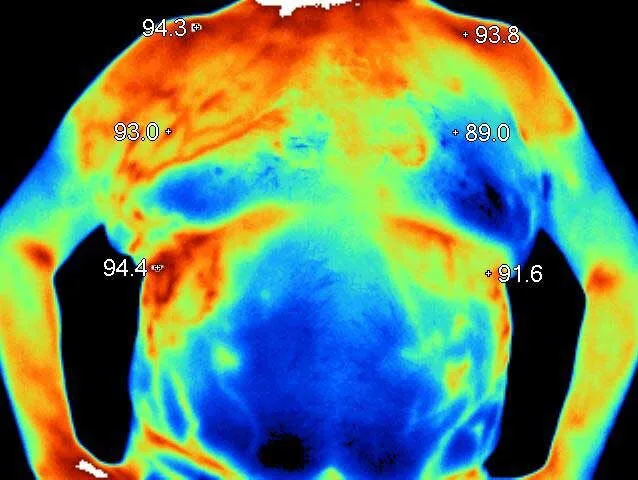
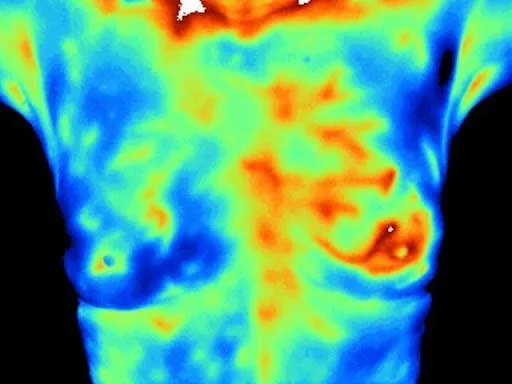
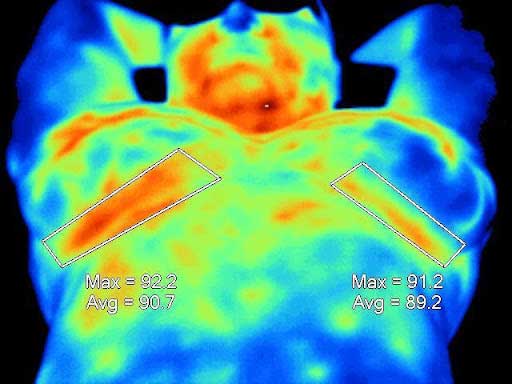
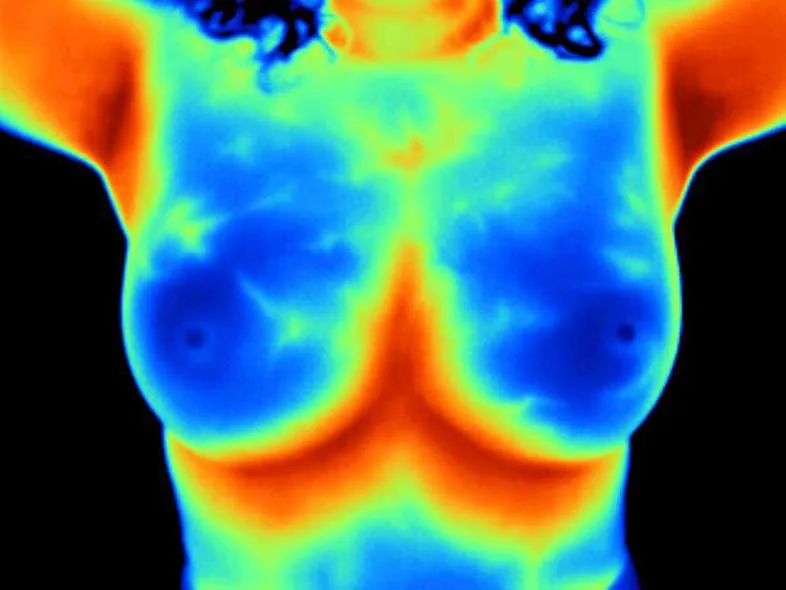
Thermography is the science of capturing and analyzing our body’s thermal energy AKA infrared heat. We cool your body slightly before the examination to highlight the heat contrast between normal and potentially abnormal tissues. Then, an infrared camera maps heat variations on your body’s surface, revealing subtle cellular changes and potential health issues long before they become major concerns. Thermography is non-invasive, radiation-free, and provides insights undetectable by MRI and X-ray.
Why Thermography?
Thermography offers multiple benefits:
What Can Thermography Detect?
Thermography can help detect a range of health issues that are closer to the body’s surface:
Early Warning of Breast Cancer
One in eight women will develop breast cancer. Thermography may reveal a developing tumor up to ten years before it is visible on an X-ray. Research has shown that adding thermography to a woman’s regular breast check-up routine leads to a 61% increase in detection rates. Furthermore, by incorporating thermography into the screening routine, up to 98% of early-stage breast cancers can be detected.
Did you know?
Is Thermography Right for You?
Thermography is a valuable addition to health screening routines for both men and women. For women, it’s an excellent tool for early breast cancer detection and is highly recommended for young women to establish baseline thermographic breast patterns starting as young as age 20. It’s also particularly beneficial for those with concerns about radiation or discomfort during mammograms.
Why Choose MyHealth1st for Thermography?
At MyHealth1st, we deliver high-quality, reliable thermography procedures:
Building on emerging clinical research, our thermography services now include a tumor marker trio – AFP, CA 153, and CEA – offering a more comprehensive assessment of breast health and significantly improving early diagnosis.
AFP, a unique fetal serum protein, is a valuable asset in breast cancer screening. It aids in early detection, significantly enhancing the accuracy of our assessments.
CA 153, with an impressive specificity of 96.43%, is a cornerstone in breast cancer screening. Its reliability in distinguishing cancer patients from those with benign conditions is well-documented.
CEA, a broad-spectrum tumor marker, is instrumental in evaluating the curative effect, condition, and prognosis of breast cancer.
This panel achieves a remarkable sensitivity of 83.46% and an accuracy of 80.25% in detecting breast cancer, as showcased in a recent study published in Frontiers in Oncology. We encourage our patients undergoing thermography to measure these labs for a more complete view of their breast health.
Discover how thermography can enhance your well-being. Contact us today to learn more or to schedule your appointment.

Join our newsletter for health news and My Health 1st events.