Breast cancer remains a leading concern for women worldwide, and early detection is crucial for improved outcomes. Mammography has long been the standard screening tool, but recent studies raise concerns about its potential role in overdiagnosis and overtreatment. This blog post delves into these issues and explores thermography as a promising screening tool for women.
In February, 2014, the Swiss Medical Board issued a disruptive report. After reviewing all the available evidence, they recommended against systematic mammography screening programs. The independent body highlighted the limitations of mammography, particularly its tendency to detect slow-growing tumors unlikely to cause harm within a woman’s lifetime. This “overdiagnosis,” they claimed, can lead to unnecessary biopsies, surgeries, and radiation therapy, causing physical and emotional distress, financial burdens, and potential long-term side effects.

Mammography is an X-ray imaging technique that involves compressing the breast tissue between two plates with low-dose radiation to create structural images of the breast. The American Cancer Society currently recommends a tiered approach to screening: “Women ages 40 to 44 should have the option to start annual breast cancer screening with mammograms if they wish to do so. Women 45 to 54 should get mammograms every year. Women 55 and older can switch to a mammogram every other year, or they can choose to continue yearly mammograms.”
These guidelines highlight a significant gap in breast cancer screening: younger women under 40, who are at average risk, do not fall within the recommended screening parameters. This leaves a considerable portion of the population without a routine, recommended method for early detection, underscoring the need for a more inclusive approach to breast health monitoring.
As we delve deeper into the research and discussions surrounding mammography, it’s crucial to weigh the American Cancer Society’s guidelines against the emerging concerns and findings from recent studies. These concerns not only question the efficacy of widespread mammography screening but also bring to light the complex balance between benefit and harm in cancer detection practices.
Multiple studies support the concerns raised by the Swiss Medical Board report. A 2020 JAMA Oncology meta-analysis revealed that for every 1,000 women screened with mammography, only 3-5 lives are saved, while 200 experience false positives and 7-10 undergo unnecessary biopsies. This translates to a false-positive rate of 20%, potentially leading to unnecessary anxiety, invasive procedures, and medical harm.
Another 2022 study in the British Medical Journal suggests even higher overdiagnosis rates, ranging from 30-50% in some populations. This raises significant concerns about the potential harms of mammography, particularly for women with low individual risk of aggressive breast cancer.
Adding to this, a critical study from the Netherlands, conducted between 1989 and 2012, found no significant decrease in the incidence of stage 2-4 breast cancers among women aged 50 and above. This finding indicates that, despite widespread mammography screening, there hasn’t been a notable impact on the detection of more advanced, potentially life-threatening breast cancers. Such results cast doubt on the efficacy of mammography in reducing the burden of serious breast cancer cases.
Moreover, the same Dutch study highlights the extent of overdiagnosis caused by mammography, particularly with the advent of digital mammography. Between 2009 and 2011, a staggering 51% of in situ tumors and stage 1 cancers in women aged 50-74 were deemed overdiagnosed. This suggests that more than half of the cancers detected through screening might not have necessitated medical intervention, leading to unnecessary treatments and associated harms.
One of the most significant issues with mammography is its high sensitivity to Ductal Carcinoma In Situ (DCIS), often marked by calcium deposits. Mammography’s ability to detect these deposits, akin to its capacity to identify bone structures, leads to a marked increase in the diagnosis of DCIS. The Netherlands study highlights a sixfold increase in the incidence of in situ cancers, including DCIS, among women aged 50-74 due to mammography screening. This substantial rise in DCIS detection is a concern, as it often leads to overdiagnosis and overtreatment. DCIS, particularly in its less aggressive forms, may not pose a significant threat to a woman’s health, yet its detection via mammography often triggers a cascade of medical interventions.
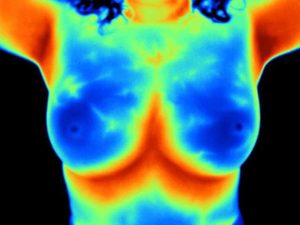
Thermography uses infrared imaging to detect variations in skin temperature, which can be associated with changes in blood flow and tissue metabolism. These changes can occur early in the development of cancer, potentially offering a window for early detection before tumors become visible on mammograms.
Thermography offers numerous benefits, including:
However, it’s important to remember that thermography is not a replacement for diagnostic procedures like biopsies. It should be used in conjunction with other screening methods, guided by a healthcare professional.
The conversation around breast cancer screening is evolving. Understanding mammography’s limitations and exploring alternatives like thermography empowers women to make informed decisions about their health. By weighing the benefits and drawbacks of each approach, women can choose a screening strategy that aligns with their individual needs and preferences.
Curious to learn more about Thermography? For a deeper understanding, we invite you to explore our Thermography Service Page. If you’re considering the service, please contact us to schedule an appointment.
References:

Join our newsletter for health news and My Health 1st events.